Immunotherapy is sometimes referred to as a type of biotherapy or biological therapy, a treatment that uses or replicates substances that are derived from living organisms. Immunotherapy uses the body’s own immune system to fight cancer cells. It can also be used to help control side effects from other cancer treatments.
Immunotherapy uses substances, or variations of substances,that naturally occur in the body to alter the functioning of the immune system so that it better identifies and kills cancer cells. Because immunotherapy uses naturally occurring substances and can be focused to identify aspects that are unique to the tumor, it can lessen the side effects of cancer treatments and help the body replace normal cells that have been damaged or destroyed. This may also help prevent the spread of cancer cells in the body. For a kid-friendly visual overview of immunotherapy, please watch our video.
How Does Immunotherapy Work?
The immune system is a network of organs and cells that work to protect the body against disease. The immune system looks for cells that are not normal, such as bacteria, viruses, and cancer cells, and tries to destroy them. Because cancer develops from one’s own cells and cancer can develop mechanisms of evading the immune system, the immune system’s response to cancer often needs a boost to assist it in better identifying cancer cells and destroying them.
During immunotherapy, patients are given substances called biological response modifiers (BRMs). These BRMs are substances that the body normally creates to fight cancer and other diseases. BRMs enhance the body’s natural ability to fight disease and boost the body’s power to recognize and destroy cancer cells. BRMs can also change the way the body reacts to a tumor.
There are two primary ways that BRMs work in immunotherapy:
- Active Immunotherapies – Stimulating the body’s natural immune system responses to work harder and more efficiently and
- Passive Immunotherapies – Giving substances, such as man-made proteins, to supplement a patient’s immune system to help it work more effectively.
The immune system can be activated against cancer cells in several ways. The most prominent immunotherapy modalities include:
- Immune checkpoint inhibitors – types of drugs that turn off the function of proteins that keep immune responses in check and can keep immune cells from killing cancer cells. When immune checkpoint inhibitors are used, they release the “brakes” on the immune system, enabling immune cells to better kill cancer cells.
- Adoptive cell therapy – a treatment where a particular type of cell in the immune system, T cells, are collected from a patient and grown in a laboratory under conditions that enable them to better recognize cancer cells when they are returned to the patient’s body. CAR T-cell therapy is a type of adoptive cell therapy.
- Therapeutic antibodies – treatment that uses proteins made by the immune system that bind to specific markers on cells (antibodies) to target tumors for destruction. Antibodies can either kill cancer cells directly, block development of blood vessels that provide the tumor with oxygen and nutrients, or help the immune system identify and kill the cancer cells.
- Therapeutic vaccines – in the same manner that an influenza vaccine primes the immune system to identify the flu virus, vaccine therapy is a type of treatment that uses substances that are specific to the tumor to stimulate the immune system to destroy the tumor cells.
- Immune-modulating therapies – treatment that either suppresses or stimulates the immune system to help the body fight cancer.
CAR T-cell Therapy Overview
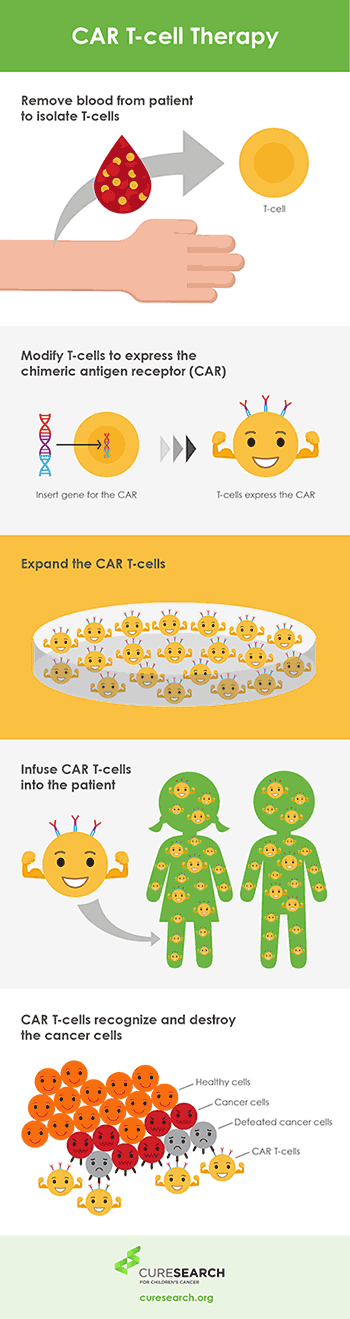 |
CAR T-cell therapy is a treatment in which a cancer patient’s own T cells are removed from his or her body and taken to a laboratory to be changed so that they seek out and attack cancer cells. Researchers add a DNA sequence to the immune cells that causes them to express a protein on their surface (a receptor). This binds them to a certain protein on the patient’s cancer cells.
The CAR T-cells are carried through the patient’s circulation and, when they come in contact with the protein on the tumor that they have been designed to identify, they mount an immune response against the patient’s cancer, eliminating the cancer cells.
PERFORMING IMMUNOTHERAPY
Immunotherapy is most often given in addition to other cancer treatments such as chemotherapy. Treatments are generally injected into a vein through an IV, but there are also pills and shots that can be given at home.
The side effects depend upon the type of treatment performed. It is common for patients treated to get flu-like symptoms. Side effects generally go away at the end of treatment.
Common side effects:
- Changes in blood pressure
- Chills
- Diarrhea
- Easy bruising or bleeding
- Fever
- Loss of appetite
- Muscle aches
- Nausea
- Skin rash
- Vomiting
- Weakness
For additional information about the immunotherapy that your child may be receiving, consult the consent forms you received before treatment started. For further information on new treatments being developed, go to www.clinicaltrials.gov.
Additional immunotherapy video and e-book resources are available: