Diagnosing Liver Cancer
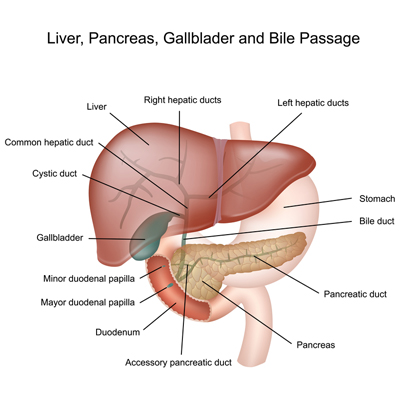
A number of tests are performed to evaluate liver cancer in a child. The first test is usually an X-ray or ultrasound. Other tests that may be performed include:
- CT scan
- Magnetic Resonance Imaging (MRI)
- Biopsy
- Blood tests
- Serum tumor marker tests
- Liver function tests
Determining Extent of the Disease
After a liver tumor is diagnosed, doctors need to assess how advanced the tumor is. This process is called staging the tumor. There are four stages of liver cancer.
- Stage I: The entire tumor was removed with surgery.
- Stage II: Tumor cells are found close to the margin of normal liver tissue after the tumor has been removed with surgery. This means that there probably are a few tumor cells still left in the liver, called microscopic residual disease.
- Stage III: Some of the tumor was removed with surgery, but some (or all) of the tumor could not be removed.
- Stage IV: The tumor has spread to the lungs or other parts of the body.
- Recurrent: The cancer has come back (recurred) after it has been treated. Liver tumors may recur in the liver or in other parts of the body.
Causes of Liver Cancer
It is unclear exactly what causes liver cancer, but researchers know that it develops due to mutations in liver cells. These cells grow without the usual regulation that tells liver cells when to replicate and when to stop replicating. When cells replicate without regulation, they can become a tumor. Some children are diagnosed with hepatoblastoma so young that scientists believe the cancer starts before the children are born. HCC is seen more frequently in areas of the world that have high rates of hepatitis. Infection with any one of several viruses that cause hepatitis is believed to be responsible.
Only a few risk factors for hepatoblastoma are known for sure. Children with some genetic syndromes are more likely to develop hepatoblastoma than other children. These syndromes are Beckwith-Wiedemann syndrome and Familial Adenomatous Polyposis. These syndromes are rare and require other medical care, and they account for only a small fraction of cases. Babies with low birth weights (less than 1,500 grams or about 3 1/2 pounds at birth) have a much higher risk of hepatoblastoma compared to normal weight babies. Smaller than average babies (3 pounds 5 ounces – 5 pounds 8 ounces) have a slightly increased risk of developing hepatoblastoma. The reasons for the high risk associated with lower birth weights are not clear. Most children who are born with low birth weight never develop hepatoblastoma.
HCC is more common in males compared to females. Hepatitis B virus passed from mother at childbirth is a HCC risk factor. Other risk factors for HCC include inherited metabolic disorders such as hereditary tyrosinemia, alpha-1-antitrypsin deficiency, disorders that lead to bile accumulation in the liver (such as Alagille syndrome) and glycogen storage disease. Obesity, hereditary hemochromatosis (too much iron accumulation in the body) and Wilson’s disease (too much copper accumulation) can also lead to liver damage and HCC.