Diagnosing Osteosarcoma
If doctors suspect your child has a bone tumor, it is important that the child is diagnosed and treated by a team experienced in working with children with cancer. Most doctors will begin by taking an X-ray of the bone. Following an X-ray, doctors may also recommend other imaging tests such as an MRI to better define the location and size of the cancer, and identify whether other structures around the bone are affected.
In addition to imaging tests, doctors will also perform a biopsy. During the biopsy, a piece of the tumor is removed and is examined under a microscope by a pathologist. Biopsies must be performed by an experienced surgeon specializing in bone and who has knowledge of bone cancers, called an orthopedic oncologic surgeon, to assure that the appropriate biologic tests are done on the sample and that the biopsy does not interfere with future surgical planning.
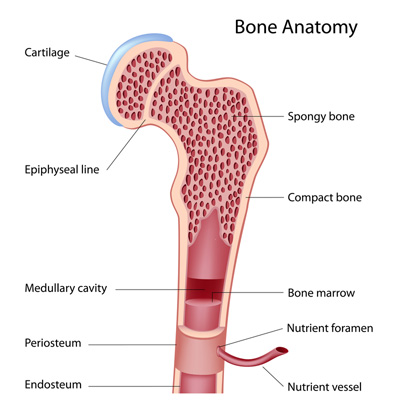
Osteosarcomas are described by their location: central tumors arise inside the bone while surface tumors arise on the outer surface of the bone. Each type has a number of subtypes. Conventional central osteosarcomas account for the vast majority of osteosarcomas in children and adolescents.
Before treating osteosarcoma, doctors need to know exactly how much of the cancer is present in the body both at the site of the tumor and elsewhere in the body. To evaluate this, a variety of tests may be performed, including scans of other parts of the body to see if the tumor has spread. The most common sites for osteosarcoma to spread are the lungs and other bones, which can be evaluated by a CT scan of the chest and a bone scan, respectively.
Types of Osteosarcoma
Doctors use the following terms to describe osteosarcoma and develop treatment plans:
- Localized: the tumor is limited to the bone of origin and the tissue surrounding the tumor; it has not spread to other parts of the body.
- Metastatic: the tumor has spread from its original site in the bone to other parts of the body.
- Recurrent: the tumor has come back after treatment. It can recur in the same place that it started, or in another part of the body. The lungs and bones are the most common sites of recurrent tumors.
- Initial response to therapy: an important prognostic (predictive of treatment success) factor is the patient’s response to initial therapy. Patients whose tumor cells have nearly all been eliminated after the initial 10 weeks of chemotherapy have a better outlook than those whose tumor cells do not respond as well to treatment. Investigators are working on finding biological differences that distinguish responsive from unresponsive tumors. If this can be determined at the time of diagnosis, treatment could be better tailored and could potentially improve the outlook for patients with less responsive tumor types.
Causes of Osteosarcoma
Osteosarcoma is likely caused by a combination of genetic changes that together cause immature bone cells to become cancer cells instead of developing into bone. The same gene that is commonly abnormal in patients that develop eye tumors called retinoblastoma (the RB gene) may also be associated with osteosarcoma. The RB gene is a “tumor suppressor” gene that normally controls the growth of cells. When it mutates, it can no longer control cell growth and tumors can form. Defects in another tumor suppressor gene, p53, can also predispose individuals to osteosarcoma and other cancers. These gene disturbances are very rare.
Despite this information, only a few risk factors for osteosarcoma are known for sure.
-
- Ionizing radiation (X-rays): There is an increased risk following radiation treatment for a previous cancer. Children who receive X-rays to diagnose a medical condition, such as a broken bone or tooth decay, are NOT at increased risk.
- Genetic syndromes: Children with some genetic syndromes caused by mutations in known genes are more likely to develop osteosarcoma than other children. The syndromes are hereditary retinoblastoma (RB gene mutations), Li-Fraumeni syndrome (p53 gene mutations) and Rothmund-Thomson syndrome (RECQL4 gene mutations). Children with these genetic conditions are at higher risk for osteosarcoma, but these account for only a small fraction of cases.
Researchers know that the vast majority of osteosarcomas develop in people who have no other diseases and no family history of bone or other types of cancer.