Also known as a BMT, stem cell transplant, or hematopoietic stem cell transplant
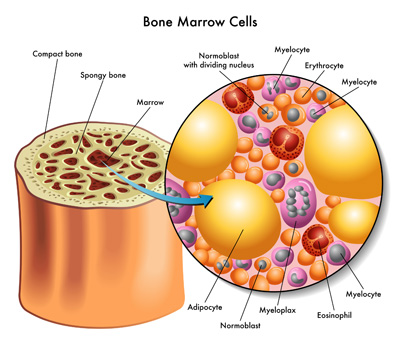 Bone marrow is found in the center of bones and is where blood cells are made. It is found in the spongy part of the bones, especially the hips, ribs, breastbone, and spine. Bone marrow contains the youngest type of blood cells known as hematopoietic stem cells. As a hematopoietic stemcell ages, it becomes a white cell, red cell, or platelet. Hematopoietic stem cells are found in bone marrow, peripheral blood (bloodstream), and umbilical cord blood.
Bone marrow is found in the center of bones and is where blood cells are made. It is found in the spongy part of the bones, especially the hips, ribs, breastbone, and spine. Bone marrow contains the youngest type of blood cells known as hematopoietic stem cells. As a hematopoietic stemcell ages, it becomes a white cell, red cell, or platelet. Hematopoietic stem cells are found in bone marrow, peripheral blood (bloodstream), and umbilical cord blood.
A bone marrow transplant (BMT) replaces diseased or damaged cells with non-cancerous stem cells that can grow healthy, new cells. BMT is usually used when cancer treatments have destroyed normal stem cells in the bone marrow. The stem cells can be replaced through BMT. A BMT is also performed when the chances for cure with chemotherapy alone are low.
Expand all sections Close all sections
There are two major types of BMT, and the type that your child will receive depends upon the diagnosis.
- Allogeneic: An allogeneic transplant is performed when bone marrow or blood cells are received from a donor other than the patient. These can come from a related donor, unrelated donor, or cord blood. This type of transplant is used for patients with leukemias and some lymphomas.
- Autologous: An autologous transplant is performed when the patient’s own bone marrow or blood cells are used. The marrow or cells are collected and frozen, and then thawed when needed for reinfusion. This type of transplant is used for patients with solid tumors such as neuroblastoma, Hodgkin disease, and brain tumors.
Allogeneic BMT
The first step is to locate a donor whose blood cells closely match the patient’s. This is done by tissue typing prospective donors. Tissue typing is done by a blood sample and is called HLA typing, which stands for Human Lymphocyte Antigens. These antigens are found on the surface of white blood cells. A patient’s full siblings each have a 25% chance of being a tissue type match. Less commonly, a parent may match the patient. Occasionally, a less- than-perfectly matched related donor is used.
If a related donor is not available, then a search for a compatible, unrelated donor is performed through the National Marrow Donor Program. Unrelated donor cells can come from a living donor or frozen cord blood. Your physician will decide what the best source for donor cells is for your child. This is based upon urgency of the transplant, weight of your child, and the best tissue type match. An unrelated donor search may take several months; cord blood can be obtained within a few weeks.
Autologous BMT
Peripheral stem cells are usually collected for autologous transplant, but stem cells from the bone marrow also can be used. These are collected either before the patient has chemotherapy or following a course of chemotherapy. To collect peripheral stem cells, the patient receives medications (such as G-CSF and/or GM-CSF) to increase the number of peripheral blood stem cells available.
Cells are collected through a process called apheresis. An apheresis machine has a circuit that will collect blood, separate, and remove white blood cells containing stem cells, and then return red blood cells to the patient. This process takes about 4 hours and may need to be repeated for 2 or 3 days in a row. For certain diseases, the peripheral blood stem cells may be treated with anticancer medications to prevent tumor cells from being placed into back into the patient’s body.
Before the transplant admission:
When the healthcare team decides that BMT is the best treatment option for your child, they will schedule a lengthy conversation with you to explain the procedure. They will explain the many risks associated with BMT, as well as what you can expect before, during, and after the transplant.
Your child will undergo testing to make sure he/she is healthy enough to withstand the rigors of transplant. Testing will include evaluation of the heart function with electrocardiogram (ECG) and kidney and liver function, and infection status. Depending upon the disease, a bone marrow aspirate and spinal tap may be performed.
When your child is deemed healthy enough for BMT, physicians will usually insert a central line catheter that allows easy access to a large vein in the chest. The catheter will be used to deliver the new stem cells, as well as blood, antibiotics, and other medications during treatment.
Preparation Before Transplant:
Your child will be given preparative treatment, called “conditioning” before the transplant. Conditioning includes high doses of chemotherapy and sometimes, radiation of the whole body. The type and purpose of conditioning depends upon your child’s underlying diagnosis but may include:
- Elimination of the cancer
- Making space in the bone marrow for new cells to grow
- Suppression of the immune system so that new cells may be accepted
Commonly used drugs include:
- Cyclophosphamide
- Melphalan
- Busulfan
- Etoposide
- Thiotepa
- Carboplatin
The Transplant
Once conditioning is complete, stem cells are given through a catheter. This is very similar to a blood transfusion. After traveling through the bloodstream to the bone marrow, the transplanted stem cells will begin to make red and white blood cells, and platelets.
It can take between 14 and 30 days for enough blood cells, particularly white blood cells, to be created so the body can fight infection. The identification of new blood cells and an increase in white blood cells following BMT is called engraftment. Until then, your child will be at a high risk for infection, anemia, and bleeding. Your child will remain in the hospital until he or she is well enough for discharge.
Outpatient follow-up is essential after discharge, as the risk of infection and other complications persist. Although the risk of relapse (recurrence of the cancer) is less with a transplant than chemotherapy, relapse may still occur. Most relapses occur within several years after a transplant.
The process of BMT places a tremendous amount of strain on the body during conditioning, the actual transplant, and in the days following transplant. Your child’s immune system will basically be eliminated during conditioning. As a result, your child will be at high risk for infection and blood-related side effects immediately following transplant. Careful monitoring, use of medicines to treat or prevent infections, and other forms of supportive care can help your child to feel as comfortable as possible.
Infection is very common before, during, and after transplant.
Anemia (low red blood cells) and thrombocytopenia (low platelets). Transfusions of red blood cells and platelets will be needed until the new cells increase sufficiently to make these.
Mucositis (sore mouth, sore throat). IV fluids or nutrition and pain medicines are used to help with these symptoms. This problem usually improves as the new cells grow in the patient.
Loss of appetite, nausea. IV nutrition and/or nutrition with a tube into the stomach are used so that weight loss doesn’t occur. Medications can be given to prevent or reduce nausea.
Infection – The patient’s immune system is destroyed after a transplant, and it takes many months and sometimes years to return. The types of infections that may occur include: bacterial, fungal, and viral. Preventive antibiotics are given for some patients. Special precautions are taken to protect your child from infection, including limiting visitors and avoiding crowded areas (such as stores) after discharge.
Graft vs. host disease (GVHD) – This occurs only in an allogeneic blood or marrow transplant. Certain types of donor cells, called T cells (or T lymphocytes) react to the patient’s body and recognize it as “foreign.” Medicines are given post-transplant to prevent this complication, but it may occur despite this.
- Acute graft vs. host disease – most commonly occurs within 3 months of transplant. The skin, liver, and intestines may be affected. Skin involvement occurs as a red rash that may be itchy or develop blisters. Liver involvement may cause jaundice or elevation of other liver tests. Intestinal involvement may cause very severe, watery diarrhea. Medicines such as steroids are used to treat GVHD and are often successful in controlling it.
- Chronic graft vs. host disease – may occur months or even years after the transplant. Most commonly it is a continuation of acute GVHD. Many different parts of the body may be affected. Skin is the most common organ affected – patients may have red, scaly skin or skin that is thickened and tough. There may also be changes in the lining of the mouth, dry eyes, dry mouth, joint stiffness, lung restriction, and difficulty absorbing nutrients from foods. In addition, patients are at risk for infection because of the medications needed to control the GVHD as well as the effect of GVHD upon the immune system.
Organ toxicity – Conditioning and prior cancer treatment may damage the lungs, liver, kidneys, and heart. These effects are unpredictable and not all children recover from organ toxicity.
Late Effects – There is a very good chance that there will be long-term effects following BMT that may not be identified until years after treatment. These include:
- Growth and other endocrine (gland) problems may develop depending upon the type of conditioning used.
- Sterility is common for most patients.
- Organ Damage can occur to the liver, kidneys, lungs, or heart.
- Cataracts may develop clouding the lens of the eye and reducing vision.